How to Reduce Claim Denials and Speed Up Medical Billing Reimbursements
Learn proven strategies to reduce claim denials and accelerate reimbursements while managing the healthcare billing services price and optimizing DME billing.
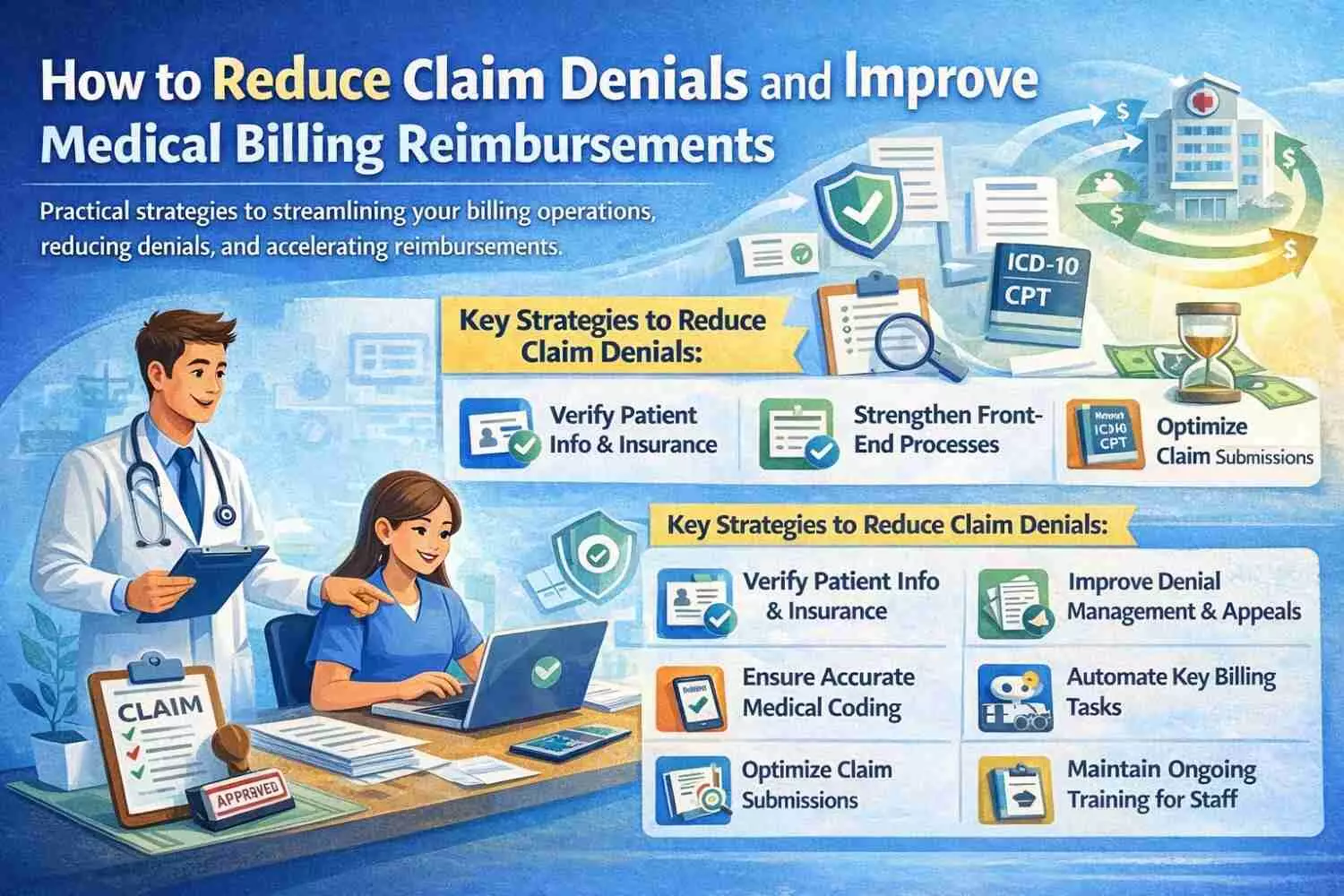
image for illustrative purpose
Medical Group Management Association statistics show that healthcare providers experience an average claim denial rate of 5% to 10%, but select medical specialties often face increased denial rates. Claim denials produce several damaging effects which including delayed revenue flow and elevated administrative obligations, and reduced practice revenue. In states like California, where
DME billing services in CA are growing rapidly, understanding how to reduce claim denials and speed up reimbursements is vital for a profitable and compliant medical practice.
In this blog, we’ll dive into practical ways to streamline your billing operations, reduce denials, improve cash flow, and keep your
cost of medical billing services under control.
1. Understand the Most Common Reasons for Claim Denials
Knowing all problem sources enables successful problem fixing. Errors in billing cycle procedures result in the majority of claim denials.
Common denial reasons include:
Incomplete or incorrect patient information
Missing or invalid authorization
Incorrect coding or modifiers
Outdated insurance coverage
Duplicate claims
Non-covered services or eligibility issues
Late submissions beyond payer deadlines
The resolution of these issues enables clinics to decrease time and financial expenses caused by mistakes.
2. Strengthen Your Front-End Revenue Cycle
Claims denial problems develop at a stage that falls before formal claim submission processes. Front-end processes need to be efficient because they stop both delays and claims denials.
Best practices include:
Insurance eligibility verification before every appointment
Accurate patient demographic entry
Pre-authorization and referral checks
Clear documentation of services provided
Collecting co-pays and deductibles upfront
Especially in billing services, where documentation and prior authorization are often required, strong front-end management can significantly impact reimbursement timelines.
3. Improve Medical Coding Accuracy
Professional coding represents both the most technological element of billing systems and a major reason why insurance claims are denied.
Tips to improve coding:
Staff members need to receive periodic training regarding changes in CPT codes and ICD-10 classification system, and HCPCS codes.
Use specialty-specific coding resources
Employ certified coders for accuracy
Providers should use double-check procedures in combination with AI-based auditing systems.
Upcoding as well as downcoding practices should be avoided because they trigger rejected payments and audits from insurance companies.
This is particularly critical when managing complex services such as billing services, where miscoding often leads to rejections or delayed payments.
4. Optimize Your Claim Submission Process
The prepared claims must move through submission systematically to prevent coding or timing-related problems.
Streamlined submission strategies:
Healthcare providers should utilize electronic claim submission through EDI whenever this option becomes available to them.
All claims need to reach payers before their established deadlines expire.
Check whether attachment and documentation specifications vary between different payer systems
Regular status checks on claims and proactive follow-ups should occur when claims experience delays.
Medical facilities should direct their claims through clearinghouses that provide error detection services before submission.
Submitting clean claims the first time around is one of the most effective ways to speed up reimbursement and lower the cost of medical billing.
5. Monitor and Analyze Denials Consistently
Ongoing quality development emerges through consistent review of denial patterns and trends.
Use analytics tools to:
Identify the top reasons for denials
The evaluation needs to divide denials between payer types and provider organizations, and specific medical procedures.
The difference between data entry mistakes and proper coding selection
Check employee performance together with their training needs evaluation
Striking the most prevalent causes of denial enables better prevention of their recurrence while improving your operational processes.
6. Enhance Denial Management and Appeals Workflow
Fast action following denied claims helps organizations secure their lost revenue amounts. An effective denial management process needs a proper structure for optimal performance.
Effective denial management includes:
The organization should use specific personnel to track down denied claims
Categorizing denials for prioritization
Appealing valid claims quickly with proper documentation
The organization must keep detailed documentation of all appealed claims alongside their status changes.
Updating payer guidelines as needed
The process reduction prevents both time losses and decreases expenses in medical billing service delivery, specifically in high-volume DME billing services within the state of California.
7. Automate Where Possible
Automation products help minimize problems and decrease both staff time and human mistakes in work processes.
Automate the following tasks:
Eligibility verification
Claim status checks
Payment posting
Remittance advice processing
Patient statement generation
Implementation of automated systems offers businesses financial savings in medical billing costs, together with accelerated reimbursement payments for all procedures.
8. Consult with a Trusted Billing Organization to Share Responsibilities
Professionals with experience in your specialty and understanding of local regulations should handle your billing operations when outsourcing proves to be your best decision.
Benefits of outsourcing:
Medical practices that work with trained coding experts and billing professionals gain access to their expertise.
Lower overhead costs
Faster claim turnaround
Compliance with evolving payer rules
Technology integration and reporting tools
Specialized DME billing service providers who master CA payer trends reduce denial rates effectively when handling billing for practices in the region.
9. Maintain Continual Training for Its Staff Members
The billing rules, together with payer requirements and coding standards, undergo regular changes. Scheduled employee training enables your organization to uphold efficient and compliant internal operations.
Include training on:
New CPT and ICD code changes
Payer policy updates
HIPAA compliance
Documentation best practices
Your staff should master the use of billing software as well as automation tools.
Funding training programs for your team will maintain their financial goal accuracy and decrease the overall expenses of medical billing services.
Conclusion: Simplify Denials and Reimbursements
With proper strategies along with expert support, healthcare providers can make claim denials reduction and reimbursement acceleration possible, even though it requires time. Enhancing front-end operations in combination with superior coding methods and automation technologies, and expert DME billing services allows healthcare providers to increase revenue flow and decrease operational expenses and medical billing costs.
The team at EASY BILLING SERVICES focuses on aiding healthcare practices to operate through complex medical billing tasks with precision and effective service delivery while following regulatory guidelines. Our team assists healthcare practices can earning faster payments along with smarter billing solutions, regardless of their present situation.
FAQs
1. What are the top reasons for claim denials?
Claim denial mainly happens because medical providers enter incorrect codes, leave essential documentation empty, or fail to secure patient authorization. Human errors that get resolved early in the process will minimize claim denials.
2. How does automation impact the cost of medical billing services?
The implementation of automation systems decreases both manual error rates and administrative work hours, which results in reduced medical billing service costs, together with speedier and more accurate claim processing.
3. Does DME billing service delivery in California differ from billing operations in other states of the U.S.?
Yes. Specialized knowledge is essential for DME billing services because following state and payer requirements directly impacts denial rates.
4. What strategies exist to monitor denial rates and lower these rates for my practice?
Analysis tools should be used to track claim rejections, followed by the creation of denial reason categories that lead to system or training changes for emerging patterns.
5. Do medical services billed through external sources yield better economic benefits than operating within the same organization?
Often, yes. Medical billing service costs decrease through outsourcing, and this process enables better claim processing and access to professional expertise and operational cost reductions.

